COVID-19 has taken the world by storm with a devastating impact on the society as well as the healthcare system. Despite COVID-19 is caused due to a virus, antibiotics are being prescribed to the COVID-19 patients, the reason being “suspecting bacterial co-infection”. In fact, studies has shown that the bacterial co-infection in patients hospitalized due to COVID-19 is only 3.5%. Low prevalence of co-infection versus the high doses of prescribed antibiotics shows the huge antibiotic misuse happening in this pandemic situation.
In this paper, 35263 COVID-19 positive patients were included spanning 154 studies. 62.4% of these patients received at least one antibiotic agent during their course of illness. The most commonly prescribed antibiotics were fluoroquinolones, followed by macrolides, beta lactam antibiotics and cephalosporins. Antibiotic prescription practice was highest in the South East Asia region (excluding China), closely followed by Middle east region, then China, North America and Europe respectively. Most antibiotics were prescribed at ICU setting while the least were in outpatient setup. The notable trend was the decrease in antibiotic prescriptions as the pandemic progressed across all regions.
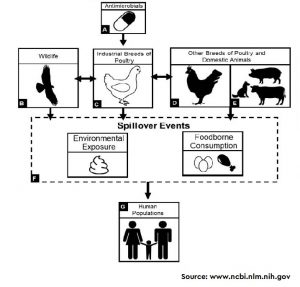
The impact of COVID-19 on global antimicrobial resistance (AMR) is uncertain. Though decreased travel, physical distancing, hospital and clinic avoidance, improved infection prevention and control, hand hygiene and environmental cleaning may decrease some of the impact of COVID-19-mediated antibiotic use on AMR, the high use of antibiotics in COVID-19 patients has the potential to exacerbate this public health threat.
To read more about the extent of antibiotic prescription in COVID-19 patients, visit the website of Clinical Microbiology and Infection (Link)