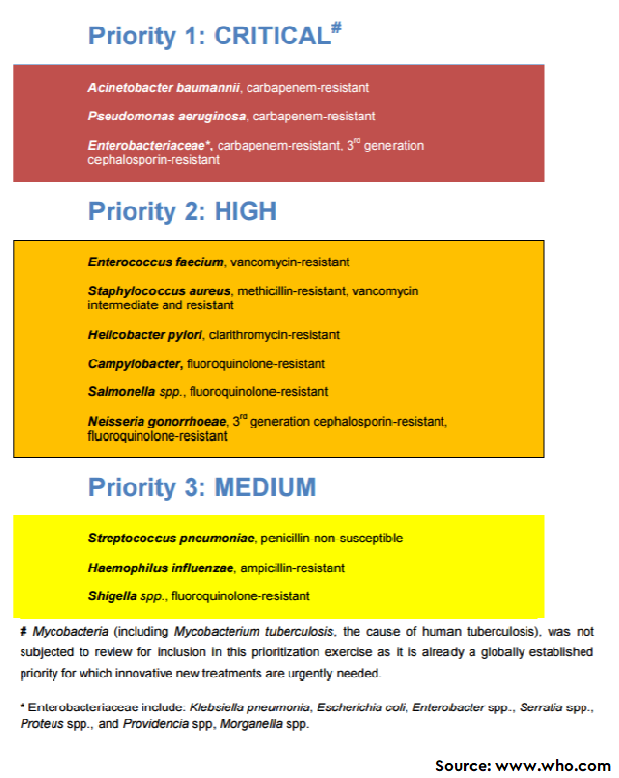
The Global Action Plan is one of the key initiatives by the World Health Organization (WHO) to combat the increasing incidence of antimicrobial resistance (AMR). In this direction, WHO has articulated a list of pathogens under the umbrella of ‘priority pathogens’ to provide strategic direction to research and develop new antimicrobials. Basically, twelve families of drug-resistant bacteria, posing the greatest threat to human health, were categorized as critical, high, and medium priority organisms, in terms of their resistance to selected antimicrobials. However, it is possible that the list varies from country to country (Link). The availability priority pathogens list at country level will direct the researchers to focus on key pathogens. Having said that, India, being one of the highest consumers of antibiotics in the world must work in this direction.
In this league, a group of scientists have tried to explore the AMR susceptibility patterns for WHO priority pathogens identified in clinical isolates collected in the Paediatrics Department of a tertiary care hospital in Southern India. Around 2000 clinical specimens, including blood, urine, stool, pus, cerebrospinal fluid (CSF), sputum, and any other bodily fluids or other clinical specimens such as catheter, umbilical, and central line tips were collected every year for culture tests. The standard methods of Kirby-Bauer disk diffusion method and/or by BD phoenix automated system were used for performing antimicrobial susceptibility patterns and reported according to standard (Clinical Laboratory Standards Institute—CLSI) guidelines. The antibiogram reports generally covered the following antimicrobials: Carbapenem, Chloramphenicol, Cotrimoxazole, Nitrofurantoin, Piperacillin, Piperacillin-Tazobactam, Tetracyclin, Tigecycline, Aztreonam, Amikacin, Gentamycin, Tobramycin, Ciprofloxacin, Levofloxacin, Norfloxacin, Cefoperazone, Ceftriaxone, Cefotaxime, Ceftazidime, Cefepime, Cefazolin, Cefuroxime, Cefoxitin, Imipenem, Meropenem, Polymyxin B, and Colistin.
Out of 12,256 culture specimens, 2335 (19%) showed culture positivity having the presence of priority list of pathogens in 1556 specimens. Results showed the presence of 72% of E. coli and 63% of Klebsiella spp. resistant to 3rd generation cephalosporins due to extended-spectrum beta-lactamase (ESBL), and 53% of the Staph. aureus to Methicillin. Overall, nearly half of Enterobacteriaceae were resistant to carbapenem (46%) or 3rd generation cephalosporins due to ESBL (55%). The carbapenem resistance in Pseudomonas aeruginosa was found low (5%). While three of the WHO ‘High priority’ pathogens and one of ‘Medium priority’ pathogen, Haemophilus influenzae (ampicillin-resistant), was not observed in this study. In conclusion, it seems that large health facilities must monitor their data to guide local priorities, policy, and practices for the optimal use of antimicrobials and better health outcomes.
To learn more, please visit the website of Scientific Reports (Link)