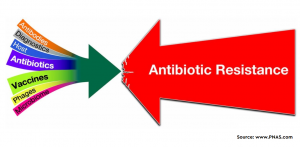
The injudicious use of antibiotics stands as the number one reason for the development and spread of antibiotic resistance in humans. This is further intensified due to the human behaviours which are intensely intertwined with antibiotic use and practices. Inappropriate prescription of antibiotics by the healthcare professional is an issue. Before jumping in to correct it, it is imperative to understand the underlying complexities of antibiotic prescribing behaviour. This systematic review and meta-ethnography bring out those grey areas.
Although, antibiotic stewardship is the responsibility of all healthcare providers, in many hospitals the antibiotic decision is taken up by senior clinicians. Junior doctors are hesitant to challenge this decision. Fast-paced clinical environments, handover errors, poor documentation, present further challenges. In an uncertain clinical situation, the short term individual costs are weighed up against long term societal gains like ABR prevention. Mostly, the clinicians perceive the threat of ABR as a distant one.
Some clinicians prescribe antibiotics regardless of whether it is evidence-based or not. This behaviour is driven by the desire to improve the condition of the patient. It acts as a confirmation to the bystanders that at least something has been done. Additionally, the priorities of clinical teams would be diverse, which also influences prescription behaviour.
The article beautiful summarises and successfully works out the complexities of antibiotic prescribing behaviour. The above-mentioned points are just a few.
For more information, please visit the website of Archives of Public Health journal (Link).