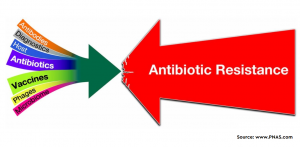
The use of antibiotics in healthcare settings is very common and it is more critical in a conditions like intensive care unit or in case of immunocompromised patients. The physicians need to prescribe the antibiotics sometimes to treat the primary bacterial infection/s or at times to avoid any secondary condition. COVID-19 is one such example of the latter scenario. Literature has shown that there has been huge dispense and use of antibiotics during the early onset of COVID-19 and most of the times, the focus was to avoid any other bacterial infection. It is well known that misuse of antibiotics further contributing to the condition named as antibiotic resistance (ABR) wherein the bacteria adapt to survive even in the presence of antibiotics. Thus, it becomes imperative to have a check on this situation. In this regard, a recent study has made an effort to find the widespread and irrelevant use of antibiotics in hospitals and local clinics is the leading cause of AMR.
The study was conducted in a tertiary care hospital to find out the prevalence of bacterial infections and AMR rates in COVID-19 patients admitted in surgical intensive care units (SICUs). The antibiotic senstivity test was conducted on the using standard Kirby Bauer disk diffusion method. The results showed that most common pathogens were E. coli (32%) and K. pneumoniae (17%). Most of the isolated E. coli were resistant to Ciprofloxacin and Ampicillin while K. pneumoniae were more resistant to Ampicillin and Amoxycillin. It was seen that most of the patients in ICU consumed carbapenem, fluoroquinolones, aminoglycoside, and quinolones. The current study provides valuable data on the clinical implication of antibiotics consumed by COVID-19 patients and AMR. Further, it was observed that most common diagnosed comorbidity was chronic kidney disease (CKD), along with urinary tract infection (UTI) (21.4%), which was caused mainly by similar organisms i.e. E. coli followed by K. pneumoniae. The most common death rate among COVID-19 patients with different comorbidities was the CLD cases, followed by pneumoniae, UTIs, sepsis, cellulitis, pancreatic cancer, ascites, CKD, pyelonephritis rigours, cystitis and hematuria.
To learn more, please visit the website of Antibiotics (link).